Abstract
Background: The impact of second line therapies on health related quality of life (HRQoL) and fatigue in pediatric patients with ITP is not well studied.
Objective: To describe the impact of second line therapies on HRQoL and fatigue in North American pediatric patients with ITP.
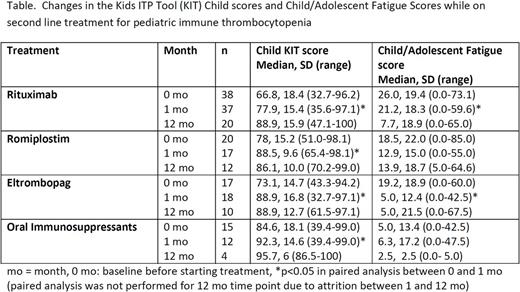
Methods: A longitudinal observational cohort of 120 children with ITP starting second line treatments was enrolled from 2013-2015 at 21 ICON centers. Enrollment requirements included age 1-17y and starting a second line treatment (not IVIG, corticosteroids or anti-D immunoglobulin) as monotherapy. HRQoL (Kids ITP Tool - KIT) and fatigue (Hockenberry Fatigue Scale - FS) surveys were completed prior to starting treatment (baseline) and 1 and 12 months after starting treatment by patient/caregiver. KIT is scored from 0 (worst) to 100 (best), and the FS scores were re-scaled so that 0 is no fatigue and 100 is highest fatigue. At the same time points as the patient/caregiver surveys, physicians assessed the perceived effect of treatment on patient HRQoL using a 7-point scale. ANOVA was used to compare the baseline means of the treatment groups. This study specifically compared change from baseline to 1 month in the KIT and FS using paired t-tests within each treatment group. The 12 month timepoint was not used in the paired analysis of individual treatments due to attrition between 1 and 12 months.
Results: The median age at enrollment was 11.3 y (1.2-17.8), and 16% (19/120) had newly diagnosed ITP, 31% (37/120) had persistent ITP, and 53% (64/120) had chronic ITP. The median number of prior treatments was 3 (range: 1-9). Fifty-eight (48%) patients had received at least one prior second line treatment. Treatments selected for second line treatment included: rituximab (n=43), romiplostim (n=31), eltrombopag (n=20), oral immunosuppressants (n=19), splenectomy (n=4), and dapsone (n=3).
The child and parent proxy KIT scores significantly improved on rituximab (p<0.001 for both), oral immunosuppressants (p=0.02, p=0.001), and eltrombopag (p=0.01 for both). Child KIT scores also significantly improved on romiplostim (p=0.003); however, there was no significant change in the parent proxy score (p=0.29). The parent impact KIT scores significantly improved from baseline to 1 month on all treatments (p<0.001), although the scores were not significantly different between treatment types (p=0.67). Child, parent proxy, and parent impact KIT scores significantly increased between 1 month and 12 months in paired analysis combining treatments (p<0.001).
As previously described, at enrollment, physicians reported that ITP had impacted the patients' HRQoL severely in 15%, significantly in 45%, moderately in 38%, and almost not at all in 3%. Physicians reported that HRQoL improved in 68% (range: 64-75%) of patients while on treatment from baseline to 1 month with no significant difference by treatment group (p=0.46). The physician's assessment of the patient's baseline HRQoL significantly correlated with the child and parent proxy KIT report (p<0.0001); however, after 1 month of treatment, the physician's assessment no longer correlated with the child (p=0.26) or parent proxy KIT report (p=0.11).
At enrollment, the median FS-Child score (n=54) was 18.5 (range 0-85), the median FS-Adolescent score (n=42) was 20.2 (0-73), and the median FS-Parent (n= 100) score was 35 (7-81). One month FS-Child improved for those who were treated with rituximab (p=0.03); there was no significant change in fatigue on the other treatments. One month FS-Parent significantly improved for those treated with rituximab (p=0.015) and eltrombopag (p=0.009).
Conclusions: In this pediatric cohort, all second line treatments appear to significantly improve HRQoL in ITP. Rituximab had the greatest impact in decreasing fatigue at one month. Physician assessment of patient HRQoL did not correlate well with patient assessment after treatment was started, suggesting there may be challenges in ascertaining the effect of treatment on HRQoL. Future analysis of ICON1 will consider the impact of treatment on HRQoL and fatigue while also accounting for the treatment effect on bleeding and platelet count.
Grace: Agios: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding. Klaassen: Amgen: Consultancy; Hoffman-La Roche LTD: Consultancy; Octapharma: Honoraria; Baxalta: Honoraria; Biogen Canada LTD: Consultancy; Agios Pharmaceuticals: Consultancy. Despotovic: Sanofi: Consultancy; Schell Cooley LLP: Other: Expert witness. Bussel: Protalex: Membership on an entity's Board of Directors or advisory committees, Research Funding; Momenta: Membership on an entity's Board of Directors or advisory committees; Rigel: Membership on an entity's Board of Directors or advisory committees, Research Funding; Novartis: Membership on an entity's Board of Directors or advisory committees, Research Funding; Amgen: Membership on an entity's Board of Directors or advisory committees, Research Funding. Rothman: Pfizer: Consultancy; Agios Pharmaceuticals: Honoraria. Haley: Genentech: Honoraria; Baxalta: Honoraria; CSL Behring: Honoraria. Neufeld: Octapharma: Consultancy, Honoraria; Genentech: Consultancy, Membership on an entity's Board of Directors or advisory committees; Novartis: Membership on an entity's Board of Directors or advisory committees. Lambert: Educational Concepts in Medicine: Honoraria; Novartis: Honoraria; AstraZeneca: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal